Pantyhose? Toilet paper? Coffee filters? Which materials make the best masks to stop the coronavirus?
It’s not news that health officials want everybody to wear a face mask in public as a measure to slow the spread of COVID-19.
The novel coronavirus is an extremely small particle that hitches a ride with droplets of saliva and mucus expelled through breathing, speaking, sneezing, coughing, and laughing. That’s why using simple fabrics to cover the mouth and nose of an infected person reduces the spread of the virus as it leaves their body.
But the extent to which masks prevent the virus from entering another person’s body through the airway varies. And, amidst the bombardment of online tutorials on face masks, questions abound about how to make them at home, and what materials to use.
Arguably, the one question to rule them all is how well those masks—made with t-shirts, pillowcases, coffee filters, toilet paper—will perform in sealing your nose from the coronavirus.
Even for masks that might not filter out everything, a tight fit against the face significantly lowers the chances of viral droplets making it to the airway, says Loretta Fernandez, an assistant professor of civil and environmental engineering at Northeastern.
That’s why any sort of filtering and interfacing that people can use in their masks could be highly protective. The idea is to create an efficient series of layers with bends within the fabric that make it harder for the virus to have a straight shot at a person’s nose. Every bend of that path provides more chances for the viral particles to stick to the fibers, instead of a person’s throat.
“By including a filter layer—coffee filters, toilet paper, any sort of thing in there that is safe to breathe—you’re just making the air have to follow a more circuitous route to get to your nose,” Fernandez says. “Putting a layer of nylon over improves that.”
Fernandez’s research focuses on pollutants in the environment, including harmful microscopic particles, and how they end up in the air we breathe, the water we drink, and the food we eat.
After the COVID-19 pandemic forced researchers to consider how their work could be repurposed to help with research to slow the spread of the novel coronavirus, Fernandez had a hunch. She started considering the tiny pollutants she studies and the laboratory instruments she uses.
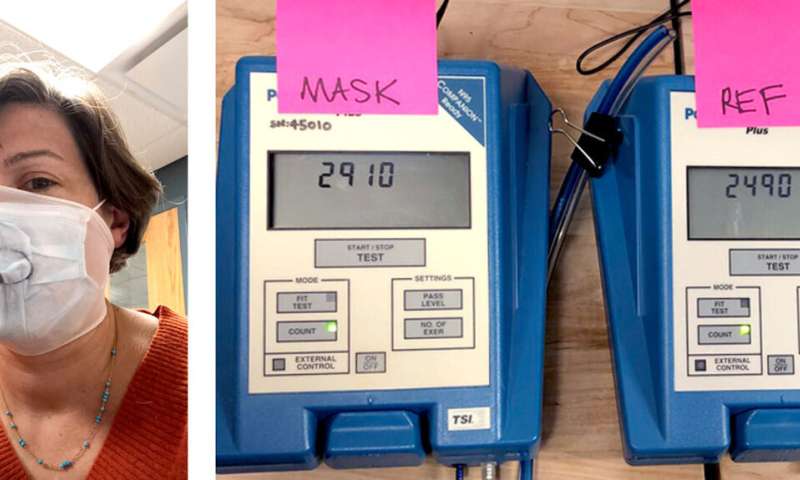
“One of them is a particulate matter counter,” she says about a machine that can analyze the concentrations of hazardous particles suspended in the air.
But particles of SARS-CoV-2, the virus that causes COVID-19, aren’t easy to count. They are as small as they are hard to catch, with a diameter several times smaller than bacterial cells. That is tiny—too tiny to be blocked by most materials in a mask without making it hard to breathe through, and too small to be detected by Fernandez’s instruments.
Still, she knew her expertise in sampling complex and microscopic particles could help. She just needed the right machine to do it.
At Northeastern, the Office of Environmental Health and Safety had started looking into university inventories, and found an old instrument that Fernandez could repurpose to count particles the size of the new coronavirus. Pfizer, the multinational biopharmaceutical corporation, also donated an instrument that served as the perfect complement to that machine.
Then, Fernandez enlisted Amy Mueller, an assistant professor of civil and environmental engineering at Northeastern, along with people and businesses in the Boston area who donated their masks.
“What’s really been the most remarkable thing is how quickly these connections formed, and how willing everyone is to share what they know, to share their equipment, and to do whatever they can to contribute,” Fernandez says.
Fernandez herself donned 10 different types of homemade masks, generated non-hazardous particles of a similar size to those that carry the novel coronavirus, and counted the amount of particles that the masks filtered.
But the instruments Fernandez and Mueller were using had not been devised to count viruses. Their software normally produces rigorous pass-or-fail assessments on whether a mask will protect firefighters from inhaling dangerous smokes and fumes.
And more than a yes-or-no answer, the goal was to determine how efficiently those masks performed, Fernandez says.
As the machines measured particles passing through the masks, they flashed values taken at every second. Fernandez and Mueller recorded those readings on video. The process required a group effort that also involved engineering students, who watched each video and paused at every second to record the data.
The preliminary results, available online, show that the most important factor to determining whether a mask will protect a person is not the material used, but how well it fits on the wearer’s face.
The tests included N95 respirators, the masks designed specifically to protect healthcare professionals who treat patients with infectious diseases, as a standard to test the efficiency of other homemade and commercial masks made with different layers of fabric, interfacing, and filters.
Commercial surgical masks performed better, filtering out about 75 percent of particles released from a particle generator located about two meters away. Homemade masks, which fit loosely over the face, generally filtered out less than 60 percent of the particles.
To improve the fit, Fernandez and Mueller wore cutouts of nylon pantyhose over the masks. That improved the effectiveness of all masks considerably, by as much as 50 percent. The idea of the nylon layer, which presses the masks closer to the face and keeps the air from circuiting around the filters, came from the past.
The early 1980s, to be specific.
John M. Price, who directs Northeastern’s Office of Environmental Health and Safety, conducted research in 1983 on methods to make homemade masks to protect people from the radioactive fallout following the Three Mile Island nuclear accident.
“We were in the laboratory trying to recreate the seal that one would get with the N95 masks by just pressing the material around the breathing zone, and Jack said, ‘you know, in the 80s, we just used pantyhose,'” Fernandez says. “The next day, we came into the lab, cut a little section to fit over the masks, and used that as a more reproducible way to hold the material to our faces.”
Fernandez says she hopes other researchers use data from her tests to study more materials and conclude which work best.
The key part, she says, is to use the results and help people at home produce the best masks they can make with whichever materials they have—as well as helping businesses put their manufacturing muscle to work.
Source: Read Full Article


