Our immune system’s capacity to mount a well-regulated defense against foreign substances, including toxins, weakens with age and makes vaccines less effective in people over age 65. At the same time, research has shown that immunotherapy targeting neurotoxic forms of the peptide amyloid beta (oligomeric Aβ) may halt the progression of Alzheimer’s disease, the most common age-related neurodegenerative disease.
A team led by Chuanhai Cao, Ph.D., of the University of South Florida Health (USF Health), has focused on overcoming, in those with impaired immunity, excess inflammation and other complications that interfere with development of a therapeutic Alzheimer’s vaccine.
Now, a preclinical study by Dr. Cao and colleagues indicates that an antigen-presenting dendritic vaccine with a specific antibody response to oligomeric Aβ may be safer and offer clinical benefit in treating Alzheimer’s disease. The vaccine, called E22W42 DC, uses immune cells known as dendritic cells (DC) loaded with a modified Aβ peptide as the antigen.
The Alzheimer’s mouse model study of this new investigational vaccine was published early online Oct. 13 in the Journal of Alzheimer’s Disease.
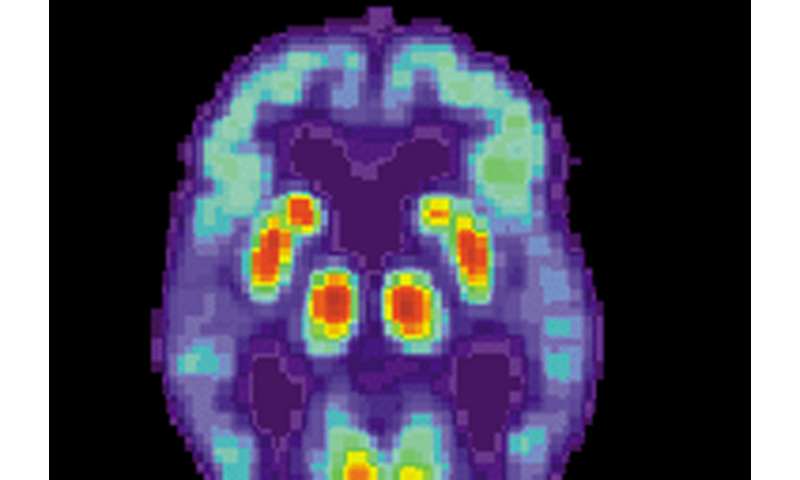
One of the two hallmark pathologies of Alzheimer’s disease is hardened deposits of Aβ that clump together between nerve cells (amyloid protein plaques) in the brain; the other is neurofibrillary tangles of tau protein inside brain cells. Both lead to damaged neurological cell signaling, ultimately causing the onset of Alzheimer’s disease and symptoms.
“This therapeutic vaccine uses the body’s own immune cells to target the toxic Aβ molecules that accumulate harmfully in the brain,” said principal investigator Dr. Cao, a neuroscientist at the USF Health Taneja College of Pharmacy, USF Health Morsani College of Medicine and the university’s Byrd Alzheimer’s Center. “And, importantly, it provides strong immunomodulatory effects without inducing an unwanted, vaccine-associated autoimmune reaction in the aging mice.”
Unfortunately, clinical trials of all anti-amyloid treatments for Alzheimer’s disease so far have failed—including the initial vaccine trial targeting Aβ (AN-1792), which was suspended in 2002 after several immunized patients developed central nervous system inflammation. “Inflammation is a primary symptom of Alzheimer’s disease, so any possible treatment with neural inflammation as a side effect essentially pours gas on the fire,” Dr. Cao said.
A next-generation anti-amyloid vaccine for Alzheimer’s would ideally produce long-lasting, moderate antibody levels needed to prevent Aβ oligomers from further aggregating into destructive Alzheimer’s plaques, without over-stimulating the immune systems of elderly people, Dr. Cao added.
In this study, the researchers tested the vaccine they formulated using modified Aβ-sensitized dendritic cells derived from mouse bone marrow. Dendritic cells interact with other immune cells (T-cells and B-cells) to help regulate immunity, including suppressing harmful responses against healthy tissues.
“Because we use dendritic cells to generate antibodies, this vaccine can coordinate both innate and acquired immunity to potentially overcome age-related impairments of the immune system,” Dr. Cao said.
The study included three groups of transgenic (APP/PS1) mice genetically engineered to develop high levels of Aβ and behavioral/cognitive abnormalities that mimic human Alzheimer’s disease. One group was vaccinated with the investigational E22W42 DC vaccine, another received an endogenous amyloid beta peptide to stimulate dendritic cells (wild-type vaccine group), and the third was injected with dendritic cells only, containing no Aβ peptide (DC control group). A fourth group was comprised of untreated healthy, older mice (nontransgenic control group).
Among the study findings:
- The vaccine slowed memory impairment in the Alzheimer’s transgenic mice, with mice in the E22W42 DC-vaccinated group demonstrating memory performance similar to that of the nontransgenic, untreated mice. In a cognitive test called a radial arm water maze, the E22W42 DC-vaccinated mice also showed significantly less errors in working memory than the mice injected with non-sensitized dendritic cells only (DC controls). Loss of working memory makes it difficult to learn and retain new information, a characteristic of Alzheimer’s disease.
- No significant differences were found in the quantities of inflammatory cytokines measured in the plasma of the vaccinated mice, versus amounts in the control mice. The researchers concluded that the E22W42 DC vaccine has “little potential for over priming the immune system.”
- E22W42 DC-vaccinated mice showed higher levels of anti-Aβ antibodies in both in their brains and in their blood than the transgenic control mice administered dendritic cells containing no modified Aβ peptide.
- Only Aβ peptides with mutations introduced in the T-cell epitope (the distinct surface region of the antigen where complementary antibodies bind) can sensitize the dendritic cells to target toxic oligomeric forms of Aβ, the researchers reported. A major advantage of E22W42 is that the antigen can stimulate a specific T-cell response that activates the immune system and silence some T-cell epitopes associated with an autoimmune response, they added.
“Though the E22W42-sensitized DC vaccine is being developed for patients with Alzheimer’s disease, it can potentially help strengthen the immune system of elderly patients (with other age-related disorders) as well,” the study authors concluded.
Source: Read Full Article
