
Obstetricians and gynecologists at Toho University, Japan examined 1,331 cases of frozen-thawed embryo transfer cycles and found that blastocysts showing shrinkage at the time of transfer had a low success rate in terms of assisted reproductive technology (ART) outcomes, demonstrating the adverse effect of shrinkage.
To evaluate blastocyst quality, ART physicians primarily use the method developed by Gardner in 1999, which is a morphological evaluation that assesses blastocoele expansion, inner cell mass, and the trophectoderm. Typically, a blastocyst with a grade of 3BB or higher was deemed a good-quality blastocyst (GQB), whereas those below 3BB were considered non-GQBs.
Although the grading system helps predict ART results to some extent, this method remains unsatisfactory, and a more accurate embryo evaluation approach is desired.
In the process called “vitrification,” one of the currently mainstream embryo freezing methods, the cytoplasm of the blastocyst is dehydrated and shrunk. This process prevents water crystallization within embryos and protects them from damage. The blastocysts are thawed at the time of embryo transfer.
During thawing, water gradually returns to the cytoplasm to re-expand the shrunken embryo. However, in some cases, when embryos are loaded into a catheter for transfer several hours after thawing, they may shrink again owing to inadequate re-expansion. Blastocyst shrinkage after thawing is known to have a negative impact on ART outcomes; however, the extent to which it has this negative effect remains unknown.
This information is of concern not only to the patient undergoing embryo transfer but also to the physician performing the procedure. The purpose of this study was to obtain accurate data on the effect of such shrinkage on ART and provide new insights into clinical practice by combining the evaluation of embryo dynamics after freezing and thawing in parallel with conventional pre-freezing morphology evaluation.
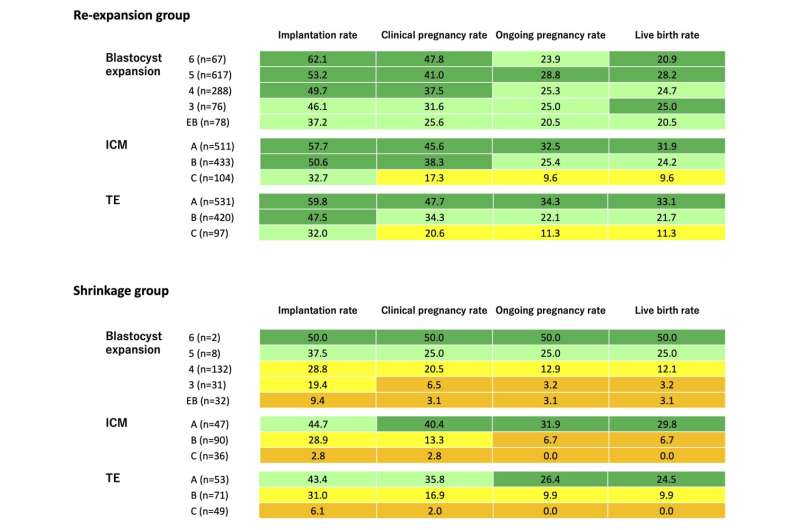
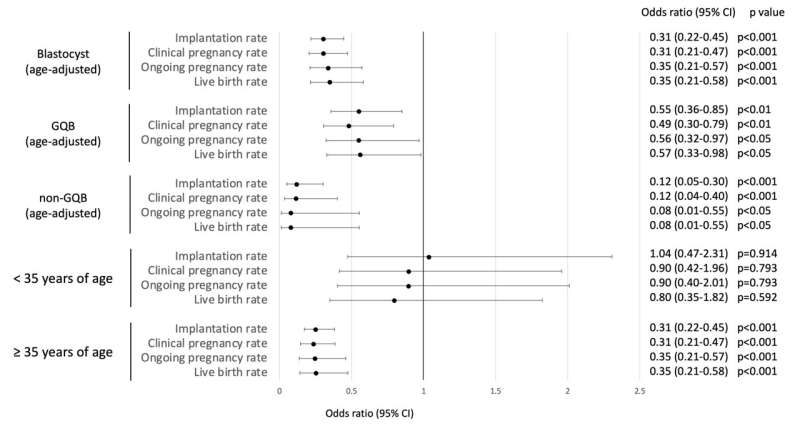
The researchers examined 999 GQBs and 332 non-GQBs that underwent frozen-thawed blastocyst transfer cycles between April 2017 and March 2022. Blastocyst shrinkage occurred in 15.4% of embryos, with the shrinkage group showing lower rates of implantation, clinical pregnancy, ongoing pregnancy, and live births than the re-expansion group. This trend persisted even when GQBs and non-GQBs were analyzed separately.
Odds ratios indicated reduced chances of success in the shrinkage group, especially for non-GQBs and women aged ≥ 35 years. A multivariate logistic regression analysis identified age, non-GQB status, blastocyst stage after day six, and post-warming shrinkage as independent predictors of clinical pregnancy.
The probability of a blastocyst shrinking after warming and recovery culturing was higher in non-GQBs, women aged ≥ 35 years, and embryos reaching the blastocyst stage after day six. The researchers concluded that post-warming blastocyst shrinkage adversely affects ART outcomes.
“In our study, we evaluated the pre-cryopreservation morphology, conducted a post-warming assessment, and summarized the outcomes. Our findings offer both patients and medical professionals a tangible reference regarding the detrimental impact of blastocyst contraction on ART results.”
“We recommend a comprehensive evaluation combining pre-cryopreservation morphology and post-warming assessment for improved embryo selection and better patient outcomes,” said Dr. Ayumu Ito, MD, Ph.D., the lead author from the Department of Obstetrics and Gynecology at Toho University Medical Center Omori Hospital. The study was published in the Journal of Ovarian Research.
Source: Read Full Article
