Expert discusses promising efforts to mitigate the opioid crisis
For the last 20 years or so, the U.S. has seen a significant increase in opioid and drug overdoses overall.
And while there was a slight leveling before the pandemic, “we’ve seen huge increases since COVID-19,” says Margaret Lowenstein, an LDI senior fellow, addiction medicine physician, and assistant professor of medicine at the Perelman School of Medicine. Overdose deaths topped 100,000 annually, setting painful records.
“Much of this is due to the rising prevalence of illicitly manufactured fentanyl, which is potent and deadly,” Lowenstein said. “We’re also seeing more stimulant-related overdoses involving drugs such as methamphetamines and cocaine.”
Some of that increase might involve people using multiple substances or drugs contaminated with fentanyl.
“We also are seeing pressed pills that contain fentanyl, [also known as] counterfeit opioids that are marketed as Percocet or oxycodone,” Lowenstein said.
Still another alarming development is the rising overdose rates in communities of color [Black and Hispanic], both in Philly and nationally. “Some of the increases are probably pandemic-related,” she said. “We’ve had social isolation, stress, economic instability, and physical illness, and we’ve also seen reduced access to services, treatment, and harm reduction.”
But a lot of marginalized people who lack access to technology lost touch with their care or returned to use during the pandemic. “It’s been a rough couple of decades, but these last couple of years have been particularly hard,” she added.
For more on possible solutions, read on.
Are there any hopeful signs on the horizon?
One big change I’m hopeful about is how the treatment system has been shaken up during the pandemic. A lot of regulatory flexibility emerged temporarily as part of the public health emergency. That allows for buprenorphine to be prescribed by telehealth and for less restrictive dispensing of methadone. The results so far are promising that these changes are largely safe and may be associated with better retention in care.
This suggests that we need more flexible models of care that are patient-centered, that aren’t punitive, that allow patients to live and work, and don’t require perfect adherence because that’s more realistic for most people. But it’s unclear how much flexibility will persist.
There’s also been some excitement in the harm reduction side. In the last year, New York City has opened overdose prevention, also known as safe injection sites, and others are considering it. Tools like Narcan distribution, syringe exchange, and fentanyl test strips are really important because people are always going to use drugs. Our drug supply is really deadly right now, and these tools help us prevent death and reduce harm. We can do a lot more.
If I have an opioid addiction, what kind of treatment would you suggest?
For opioids, there’s clear evidence that treatment with medications like buprenorphine or methadone is far more effective than any other option. There are many different models in which medication is delivered, but what’s clear is that medication is the primary thing that reduces death and improves other health outcomes. If a person wants to engage in therapy or groups, that’s great, but medication should not be delayed.
Substance use disorders are treatable conditions. But it’s common for people to return to using, especially early on. We should prepare for that. We should give people the tools to manage that like Narcan and fentanyl test strips, and not kick you out of treatment because you return to using. Addiction is a funny thing. When you display symptoms of your disease, we kick you out of care.
Can you describe your new study? What’s significant about it?
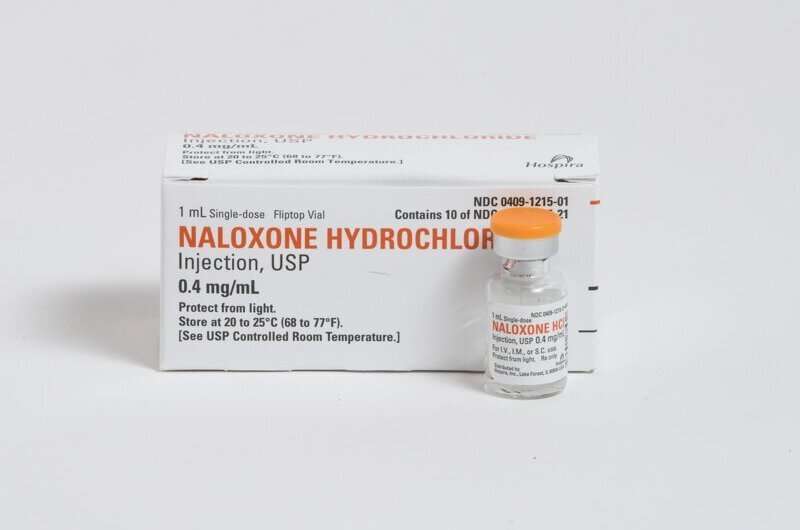
Our team interviewed patients who were seen in Penn Emergency Departments (EDs) and received a naloxone (often known by its brand name Narcan) prescription to prevent a future overdose. We wanted to assess their familiarity with naloxone and how they felt about getting it in the ED. We found one group was highly engaged in harm reduction and knew all about naloxone. “I carry it, I give it to friends,” they said. But many others had little or no exposure to naloxone and little understanding about overdose risk and harm reduction. This underscores how EDs are important places to be educating people and delivering harm reduction interventions.
Another key point: People were generally very happy to get naloxone in the ED, but a lot of them never talked to their providers about it. So there was a missed opportunity for education. We’re doing better about providing harm reduction tools, but we could do more to make sure patients understand how to reduce their own risk.
How does this study fit in with other recent work?
One of the things I’m interested in is these reachable moments for people who use drugs, like providing naloxone during an ED visit or using telehealth to prescribe medication treatment the same day patients ask for it.
The health system is not always welcoming for people who use drugs. There’s a lot of stigma and trauma, so patients often don’t want to seek out care. So how can we engage the most at-risk patients? Can we find them in the community? Can we get them in the door via telehealth? A lot of the old models are punitive and come with the outdated sense that you need to jump through hoops or reach rock bottom to get treatment. But the evidence doesn’t support that. It’s better to engage people whenever you can and do more to help the people who aren’t getting to us.
One project I’m really excited about is the CareConnect Warmline, which was started by our team at the Penn Center for Addiction Medicine and Policy in partnership with Penn Medicine OnDemand. We also have funding from the city health department and Independence Blue Cross. It’s a telehealth service that gives patients same-day access to buprenorphine. People can call the number (484) 278-1679, talk with an experienced substance use navigator, and soon get connected to a clinician. It’s one of the few ways to get same-day treatment where and when you need it. At this point, we have seen over 300 patients and prescribed medications for over 200.
What other recent work applies?
People who use drugs are spending time somewhere. There is a study from Massachusetts that looked at how many overdose victims were seen across the state’s health systems, Emergency Medical Services (EMS) calls, jails, and more. Only half the people who died of an overdose received care at any of those places. That really struck me. We are just not even seeing a lot of at-risk people.
We need to reach people in spaces outside of health care settings, wherever they spend time. I worked with LDI Senior Fellow Carolyn Cannuscio to interview public librarians about their experience with substance use and overdose, and we partnered with the city’s Department of Public Health, pre-COVID, to do library-based naloxone training for the community. Libraries are welcoming places where a lot of people go for health information. It’s an optimal spot to give Narcan training.
I also provide buprenorphine with Prevention Point, Philadelphia’s mobile overdose response unit, which brings treatment and harm reduction to areas of Philadelphia with high overdose prevalence. The idea is to lower barriers to treatment access as much as possible and get people engaged in care.
What do you wish you knew more about? Where are you heading?
I just started a National Institutes of Health (NIH) career development award focused on improving transitions of care for hospitalized patients with opioid use disorder with the goal of helping patients continue in care after discharge. With my colleague and LDI Senior Fellow Jeanmarie Perrone and Certified Recovery Specialist Nicole O’Donnell, I am also working on growing our telehealth buprenorphine program, CareConnect. And we are collaborating with LDI Senior Fellow M. Kit Delgado on a new Patient-Centered Outcomes Research Institute (PCORI)-funded study that builds on the CareConnect model to test text messaging and financial incentives for patients who start buprenorphine in the ED.
What recommendations do you have for policymakers?
We need a lot more investment in harm reduction that is sustained, both inside the health care system like in EDs and hospitals, and outside in community sites. We also need to permanently loosen restrictions around medication prescribing, including flexibility for methadone, and allow buprenorphine to continue to be prescribed by phone. We need to stop putting up roadblocks to lifesaving medication and make it easier for patients to follow up in care by implementing more low-threshold treatment models that reach the most marginalized patients. And we need to scale up treatment in jail and prisons. Release from incarceration is an incredibly high-risk time, but people rarely receive evidence-based care.
Source: Read Full Article


