A clinical trial by Menzies School of Health Research (Menzies) published in The Lancet has revealed promising results to reduce malaria relapses, through the broader use of primaquine.
Primaquine is a medication used for more than 60 years to target vivax malaria parasites in the liver and prevents infection from continuing. Usually only patients who are infected with P. vivax malaria receive this treatment.
This study assessed the use of primaquine in patients with another malaria species, P. falciparum. Those patients received one of two treatments. One group received the current recommended treatment for P. falciparum, which only targets the blood form of the parasite. The second group received this treatment as well as primaquine.
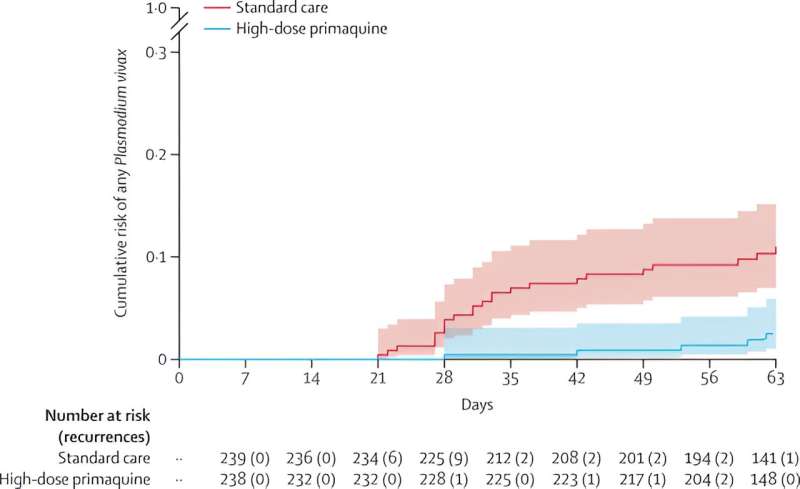
Patients who received the additional treatment had significantly fewer relapses of P. vivax. This study also provided reassuring evidence on the safety of primaquine at a higher dose than used in most countries.
Led by Menzies principal research fellow, Associate Professor Kamala Thriemer, this multi-center study was conducted in Bangladesh, Indonesia and Ethiopia.
P. vivax malaria affects more than 7 million people each year, mainly throughout the Americas, Africa and the Asia-Pacific. It puts 40% of the world’s population at risk of the infection. Once infected, P. vivax can hide in the liver for long periods of time before reappearing and causing a malaria relapse.
Locations where both P. falciparum and P. vivax are present are known as co-endemic countries. In these settings, the risk of a P. vivax relapse after a P. falciparum infection is significantly higher compared to the risk of P. vivax relapse from an initial P. vivax infection.
More people with malaria means more opportunities for the disease to be spread by mosquitos. Treating the liver forms of the P. vivax parasites at the point of care for a P. falciparum infection can contribute to improved malaria control and ultimately elimination.
These findings provide significant evidence towards new innovative ways to reduce malaria cases, supporting malaria elimination goals.
Associate Professor Kamala Thriemer says, “Malaria elimination requires wide-scale provision of safer and more effective antimalarial treatments, this is particularly the case for vivax malaria.
“We know that in areas where the two most important malaria species are present, the risk of a P. vivax relapse after a P. falciparum infection is high.
“This clinical trial found that using radical cure in patients with P. falciparum malaria has the potential to reduce the risk of future P. vivax episodes. In patients who received radical cure the risk of P. vivax reinfection was five times lower than in participants who received standard treatment.
“This provides an opportunity to treat more patients who are at risk at the point of care, ultimately contributing to better malaria control.”
Asia Pacific Malaria Elimination Network (APMEN) Vivax Working Group co-Chair Dr. Neena Valecha says, “Primaquine is safe for most patients, but the drug can induce a severe form of anemia (called hemolysis) in patients with a particular enzyme (G6PD) deficiency.
“With availability of novel diagnostic tools for point of care G6PD testing, universal radical cure can be provided safely and effectively and can help National Programs to accelerate towards the goal of malaria elimination.
“Moreover, uniform treatment for both species can be user friendly and simpler to implement.”
More information:
Kamala Thriemer et al, Primaquine radical cure in patients with Plasmodium falciparum malaria in areas co-endemic for P falciparum and Plasmodium vivax (PRIMA): a multicentre, open-label, superiority randomised controlled trial, The Lancet (2023). DOI: 10.1016/S0140-6736(23)01553-2
Journal information:
The Lancet
Source: Read Full Article
