For those fearing their memories are fading, the ads provide hope.
“Early diagnosis extends quality of life,” says an ad by Dung Trinh, an Orange County physician, on the website of a program for seniors at Mount of Olives Church in Mission Viejo.
Trinh offers free memory tests and personalized recommendations based on the results. He gives scores of lectures a year at assisted living homes, senior centers, churches and Rotary Clubs in Southern California, telling audiences how they can keep their memories sharp. He describes himself as a medical missionary and “healthy brain” expert.
All this helps in his job of recruiting patients for a private company’s clinical trials of experimental drugs for Alzheimer’s disease.
The studies Trinh is recruiting for are part of a new gold rush in pharmaceutical research that was sparked when federal regulators approved two new drugs for Alzheimer’s. Trials of those two drugs have shown at best modest results in slowing cognitive decline.
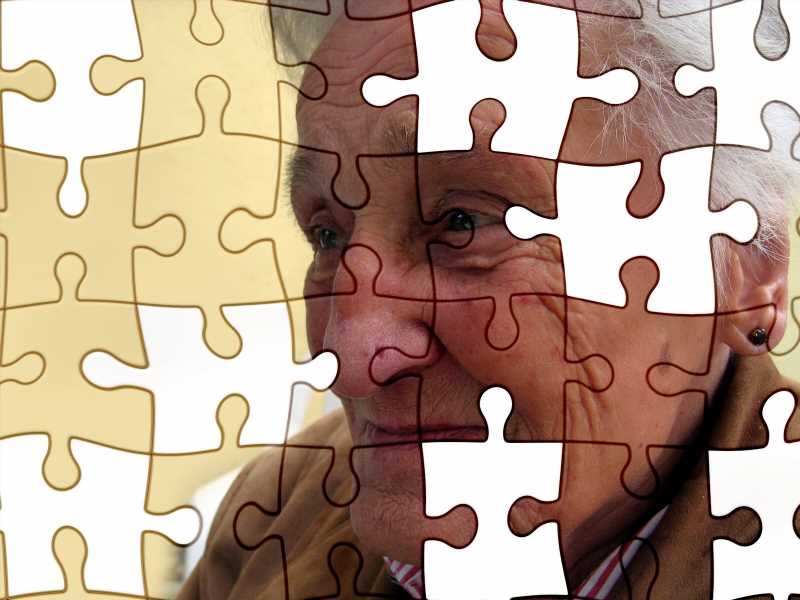
The Food and Drug Administration’s controversial approval of the two drugs—Aduhelm and Leqembi—came as the country struggles with caring for a fast-rising number of Alzheimer’s patients with no cures to help them. More than 6 million Americans have Alzheimer’s—a total expected to double in the next 25 years.
After the manufacturers priced the first two medicines at more than $26,000 for a year of treatment, other companies sped up their efforts to complete clinical trials of their experimental drugs. More than 57,000 research subjects are needed for the planned trials of more than 140 experimental drugs for Alzheimer’s disease, according to a study published in May. A drug that meaningfully improved memory function could extend the quality of life for millions of people while saving billions of dollars in healthcare costs.
The increasing sums spent to recruit older people with memory problems to these experiments gives some doctors pause. They say that people with dementia can confuse the helpfulness of clinical trial recruiters with actual medical care from doctors, an outcome that scientists call a “therapeutic misconception.” The purpose of a clinical trial is to test an experimental drug, these doctors point out, and not to provide medical care.
And the trials have been the subject of intense debate. More than 95% of the studies of dementia drugs have failed to show the therapy slows memory decline. Plus, the drugs come with adverse effects, sometimes serious. At least three people participating in trials of Leqembi died, although its maker has questioned whether the drug was the cause, saying the number of deaths was similar to the rate in the placebo group.
The two new drugs and many of the others being studied are monoclonal antibodies that are designed to clear amyloid, a protein that can build up in the brain. They are given by intravenous infusion and come with a risk of bleeding or swelling in the brain. In the trials of Aduhelm, 40% of participants suffered from brain bleeding or swelling.
Aaron Kesselheim, professor of medicine at Harvard Medical School, said scientists performing the studies need to make sure patients with memory problems understand the risks.
“This is a population that may not fully understand the consent process,” Kesselheim said. “The investigator needs to be very careful to make sure people know what they are getting involved with.”
Peter Whitehouse, professor of neurology at Case Western Reserve University, said trial investigators can “earn phenomenal amounts” for the patients they recruit.
“There’s a bias for them to want to get people into these studies,” said Whitehouse, who has studied the financial conflicts of interest in Alzheimer’s research. In some cases, he has found, “they overpromise the likely results of these trials and create false hope.”
Trinh is an executive at privately held Irvine Clinical Research, which says it “is the leading independent site” for Alzheimer’s drug trials in California. The company has long focused its recruitment efforts in Orange County, with its large retirement communities, including Laguna Woods Village, which has 18,500 residents.
Late last year, Trinh expanded the company’s reach by setting up an office in Long Beach called the Healthy Brain Clinic, where he said he hoped to reach more Black patients and other minorities.
He holds “lunch and learns” where people can get a free meal while hearing his health tips. All his services are free to the patients, he explained in a February podcast. Pharmaceutical companies eager for new study volunteers are picking up the tab, he said.
His assistant assured the podcast audience that there was “absolutely” no danger for volunteers. “The patient’s health is our No. 1 priority,” she said.
In September, an 84-year-old grandmother from Lake Forest signed herself up for a trial at Irvine Clinical Research. The woman’s daughter said she did not learn of the clinical trial until weeks later when her mother suffered a sudden decline, acting confused and unable to remember what day it was. The family took her to the doctor, who ordered an MRI, which showed she had suffered a stroke.
The daughter asked that the family not be named so she could speak openly about her mother’s medical condition and treatment. The daughter said her mother had been worried about her memory but had not been diagnosed with Alzheimer’s.
She allowed The Times to review documents from the trial of the experimental drug called remternetug, which is owned by Eli Lilly, as well as the woman’s medical records confirming the stroke.
The woman signed a 21-page consent form, which listed risks of the drug.
Her daughter said her mother had recently struggled to make sense of her monthly electric bill.
“How was it even possible for her to consent to this study?” her daughter asked.
Federal regulations say that a person without the mental capacity to understand the consent form in a trial may not be enrolled unless a legally authorized representative consents on the subject’s behalf.
The FDA recommends that scientists running the study consider having an independent monitor such as a clinician unaffiliated with the trial’s sponsor determine whether patients have the mental capacity to know the risks in the consent form.
“From an ethical perspective, you want to make sure that people understand information that’s given to them,” said Emily Largent, a bioethicist at the University of Pennsylvania.
“Even well-intentioned investigators can sometimes have a conflict of interest,” she said. “It can help to have somebody who’s looking at the situation a little bit more dispassionately to maximize protections for individuals.”
In October, the woman received the first drug infusion in the trial. When she didn’t show up for later visits, Irvine Clinical Research repeatedly sent Ubers to pick her up at her mobile home park, her daughter said, which the family sent away.
The Times spoke to the woman this month. She said she did not remember going to Irvine Clinical Research or any of the visits described in the documents. “When did I go there?” she asked.
Ralph Lee, chief executive of Irvine Clinical Research, declined to answer questions, including how his company had ensured elderly patients had the capacity to understand the consent form and whether it used an independent expert. “We keep information about clinical trial participation strictly confidential, so we cannot answer your request,” he wrote in an email.
Trinh did not respond to repeated voicemail and email messages.
Irvine Clinical Research has performed other research for Eli Lilly. The trial company’s executives wrote on LinkedIn that they had enrolled more people into studies of donanemab, Lilly’s other experimental drug for Alzheimer’s, than any other trial site in the world.
Tarsis Lopez, an Eli Lilly spokesperson, said that the drug company’s research is subject to review by an independent institutional review board, which must approve trial protocols and consent documents.
The protocol for remternetug required participants to have Alzheimer’s disease that “has not progressed beyond the mild dementia stage,” he said.
“Lilly takes the safety and well-being of our valued clinical trial participants very seriously,” he said. “We are saddened to hear when anyone participating in a clinical trial experiences challenging medical issues, but we cannot comment on the specific circumstances of individual participants in ongoing clinical trials.”
Advarra, the private-equity-backed, for-profit institutional review board that Lilly hired to oversee the trial, declined to comment.
Performing clinical trials can be a lucrative business. A study of 225 clinical trials performed between 2015 and 2017 found that it cost pharmaceutical companies an average of more than $40,000, and as much as $75,000, for each test subject completing a trial.
Trials of Alzheimer’s drugs are especially expensive, according to USC researchers, because of the difficulty in recruiting patients and the extensive testing required of each participant. Drug companies typically pay the recruiting company $600 for a cognitive test, $2,400 for an MRI and up to $8,000 for a PET scan, the researchers said. Volunteers are often compensated as well.
Pharmaceutical companies are willing to pay those sums because a drug that wins approval can bring in many billions of dollars. Eisai, the Japanese company that sells Leqembi, one of the two drugs conditionally approved by the FDA, expects worldwide annual sales of the drug to reach $7 billion by 2030, the company’s executives said in March.
The FDA initially approved Leqembi and Aduhelm under accelerated approval rules that are used for drugs greatly needed by patients but not yet backed by studies proving their potential benefits.
On July 6, the agency granted Leqembi full approval based on an Eisai study that showed the drug slowed the rate of cognitive decline by 27%. Some doctors question whether that figure, which represents less than a half-point on an 18-point scale of cognitive function, constitutes a meaningful improvement for patients.
Irvine Clinical Research is just one of dozens of for-profit companies recruiting Alzheimer’s patients in California and across the country. The pharmaceutical companies also pay universities to recruit patients, but they often turn to the private research sites where there can be less bureaucracy to navigate.
“Drug companies have found that academic institutions can be difficult to deal with,” Whitehouse said. “So they like these private operators, who basically set up their own system to do trials and can be much more efficient at enrolling patients.”
Of the 76 sites recruiting patients for Lilly’s remternetug trial, one is a university.
Parexel, a trial operator owned by two private equity funds, including one controlled by Goldman Sachs, recruits patients using a method similar to Irvine Clinical Research’s. It created what it calls “a community memory clinic” on the campus of Glendale Adventist Medical Center.
In a medical journal article about the clinic, Parexel staff explained the company was recruiting patients for the earliest human trials of experimental drugs, including Phase 1. Such trials often involve small numbers of people because little is known about the experimental drug’s effect in humans. The employees wrote it was difficult to get people to sign up for these trials because they come with higher risks and require complex invasive procedures such as lumbar punctures.
The Parexel employees wrote that they had “significantly increased” the number of people referred to the company’s clinical trials by hosting lectures for seniors and then asking audience members a series of questions on their cognitive abilities. Those who appear to suffer from memory problems are invited to the memory clinic for a battery of neurological tests, they wrote.
If the staff concludes the person has mild cognitive impairment or Alzheimer’s disease, the article said, the person and their family are given recommendations and told about available clinical trials for which they could volunteer.
Parexel told The Times in a statement that the doctors and staff operating the memory clinic were separate from those performing the clinical drug trials. “The memory clinic does not manage clinical trials, it does not administer investigational drugs,” it said.
If the clinic finds a person has cognitive decline, the company said, the results are provided to the participant’s primary care physician for a diagnosis.
“Patient safety is always the highest priority,” Parexel said.
The company said that a physician running the trial makes sure participants are competent to understand the study risks by quizzing both them and their family members about the information in the consent form. It said the physician is employed by a medical group not owned by Parexel.
Since Parexel’s memory clinic opened in 2016, more than 400 people have had cognitive evaluations, the company said, but less than 3% were deemed eligible to participate in a clinical trial.
When pharmaceutical companies pay for the clinical trials, they control what information gets released.
Eli Lilly began testing remternetug in 2018 but decided to stop the Phase 1 trial after enrolling 36 healthy adults. The company did not release the results.
Six months after the Lake Forest woman entered the trial at Irvine Clinical Research, Lilly released data on 41 participants in a second Phase 1 trial.
The company said the drug had led to “rapid and robust amyloid plaque reduction” in the subjects’ brains and that the results supported its continuing research.
A close look at the data shows that 24% of the subjects suffered brain swelling and 17% had bleeding in the brain, according to the study. One of the 41 volunteers had both brain bleeding and swelling and attempted suicide.
David Knopman, a professor of neurology at the Mayo Clinic in Minnesota, reviewed the data for The Times and noted that the cases of brain swelling and bleeding increased as test subjects were given higher doses. He described the case of the participant who attempted suicide as a “serious symptomatic adverse event.”
The question, he said, is if investigators used the same dose in 200 people, how many of them would suffer similar complications. “And then the next question is, what’s the limit for where it becomes unacceptable?”
Knopman said that while the data showed the drug reduced levels of amyloid plaque, scientists don’t know whether that leads to improvement in cognitive abilities. “They removed amyloid, but you don’t know if that had any clinical benefit,” he said. That question is still being studied.
FDA guidelines say that recruiters trying to enroll people into studies should not imply that the experimental drug is safe or effective. Recruiters also should not promise free medical treatment, the agency said.
In a May 2022 webinar for residents of the Covington, an assisted living facility in Aliso Viejo, and other senior residences owned by ECS, Trinh told the audience they could get free tests to look for amyloid plaque in their brains at his office.
“Just give a call whenever today, tomorrow,” said Trinh, after giving the audience his email address and phone number.
“If we scan your brain or if we draw your blood and we see plaque, then we have medications in clinical trials that are designed to remove the plaque,” he said. “Our goal is plaque removal before there’s significant damage because that’s where prevention comes in.”
2023 Los Angeles Times. Distributed by Tribune Content Agency, LLC.
Source: Read Full Article