Women are more likely than men to develop more-deadly right-sided colon cancer
The traditional broad categories of cancer are splintering into finer subcategories as researchers unravel the incredible complexity and variety within locational descriptors such as “breast cancer” or “lung cancer.” For instance, we now know that the general term “breast cancer” encompasses a range of heterogeneous tumors with different genetics, mechanisms, and drivers requiring different targeted therapies.
Colon cancer has been undergoing a similar subdivision. Researchers have known for years that colorectal cancer is the third most common cancer diagnosis in the United States and the second leading cause of cancer-related deaths. The National Cancer Institute estimates 149,500 new cases in 2021 and 53,000 deaths.
More recently, researchers have learned that cancers on the colon’s right-hand segment, which ascends the right side of the abdomen, differ from cancers located on the segment descending alongside the abdomen’s left. Researchers also found that these different locations led to different outcomes. People with right-sided colon cancer (RCC) had a 20 percent greater chance of dying than people with left-sided colon cancer (LCC). Subdividing further, scientists observed that left-sided cancers were split almost evenly between males and females (52 to 48 percent, respectively), but the more deadly right-sided type affected women much more—females account for 62 percent of RCCs, males just 38 percent.
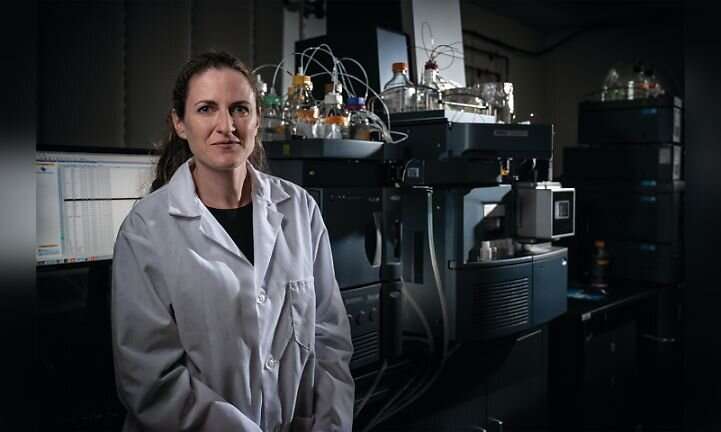
These fascinating differences beg the question: why? Why do right-sided and left-sided colon cancers differ? Why are right-sided ones more dangerous? And why do women get more of them? These questions, especially the last one, motivate Caroline Johnson, Ph.D., Assistant Professor of Epidemiology (Environmental Health Sciences) at Yale School of Public Health and a member of the Cancer Prevention and Control Research Program at Yale Cancer Center. Dr. Johnson began researching colorectal cancer as a research fellow at the National Cancer Institute and has continued that focus in her lab at Yale School of Public Health. Her focus is metabolites and their role in human health, particularly in colorectal cancer.
Metabolites are molecules formed or used during the process of metabolism. They can be produced by diet, hormones, genetic or environmental factors, and the microbiome. The study of metabolites and their interactions is called metabolomics, Dr. Johnson’s area of expertise. “Metabolites give us information about biological processing within a sample or within a tissue,” she said. “Tumors have metabolic activity and make metabolites that can produce energy for cell growth.” In the first such study ever done, she and her colleagues used metabolomics and mass spectrometry to explore the marked differences between right-sided colon cancer in males and females. The process works like this: first they extract metabolites from a tumor sample by liquefying and centrifuging it. The proteins sink, the metabolites float. The researchers run the metabolites through a mass spectrometer to get a survey of everything in the sample—perhaps 20,000 variables—which can be separated into various groups. They look for patterns and connections by putting the metabolites into a pathway analysis that reveals their links and shared networks. “We’re able to pinpoint what genes and enzymes might be altered or upregulated or downregulated in relation to the disease,” said Dr. Johnson. The researchers discovered that colorectal cancer cells on the right side generate metabolites that enable more aggressive growth in women, than in men. They also determined that the colons of males and females produce different metabolites. That insight led them to identify a distinct metabolic phenotype common among women with right-sided colon cancer. “This phenotype produces energy in a different way than happens in males,” explained Dr. Johnson.
The biggest difference is a large increase in asparagine, a common amino acid found in most proteins. “So, we looked at the gene that produces asparagine, which is asparagine synthetase (ASNS),” said Dr. Johnson, “and then we looked at many cancer databases to see if females with right-sided colon cancer have a higher expression of that gene and lower survival.” The data showed a correlation in women but not in men. “Asparagine might be involved in tumor growth in females,” said Dr. Johnson. When right-sided colon tumors become starved for energy, they look for new sources. In women, asparagine production goes into overdrive to help the tumor increase its uptake of the amino acids and fatty acids that fuel cell growth. “It’s called ‘metabolic rewiring,'” said Dr. Johnson, “almost like you rewire the electricity supply in your house. The tumor suddenly switches to using different nutrients to survive in a different situation.” Dr. Johnson’s discovery of asparagine’s role opens therapeutic possibilities. Drugs that remove asparagine from circulating blood, depriving tumor cells of fuel, are already being used against acute lymphocytic leukemia. One of Dr. Johnson’s next studies will test whether the drugs might be effective against RCCs. Using mice with colon cancer, she will remove the asparagine synthetase gene using the gene editing tool CRISPR, and then will feed the mice diets high or low in asparagine to monitor the effects on tumor growth. She isn’t sure that removing asparagine will be as effective on RCCs as it is on acute lymphocytic leukemia, since the colon is a more complex environment, including the microbiome. For that reason, she is also working on tracking the biology back toward the source before asparagine is activated.
Her research indicates that mutant KRAS genes, which are implicated in several cancers including colon cancer, play a role in asparagine metabolism. at connection is now her lab’s primary focus. “We’ve seen that mutant KRAS could be regulating the production of asparagine,” she said. “We’ve also seen that women with right-sided colon cancer, if they express mutant KRAS, have a much poorer survival. That observation was quite striking, and I don’t think it has been reported before. So, we’re trying to see if we can prevent asparagine production by targeting mutant KRAS better. We’re also looking at why mutant KRAS is regulated differently in women than in men, and what different hormones are involved. It’s a very complex signaling pathway. We need to look a little bit further upstream at that oncogene.”
Dr. Johnson notes that the connection between mutant KRAS and asparagine could have therapeutic implications. A patient with early-stage colon cancer and elevated levels of asparagine could be treated more aggressively, perhaps with hormones. The phenotype Dr. Johnson identified among women with RCC occurs in menopausal and older women.
Source: Read Full Article



