The ability of COVID-19 to infiltrate and potentially change the function of a variety of different cells in the body, including the insulin-producing beta cells of the pancreas, is the subject of a special session at this year’s Annual Meeting of the European Association for the Study of Diabetes (EASD). The presentation will be given by Dr. Shuibing Chen, Department of Surgery, Weill Cornell Medicine, New York, NY, U.S.
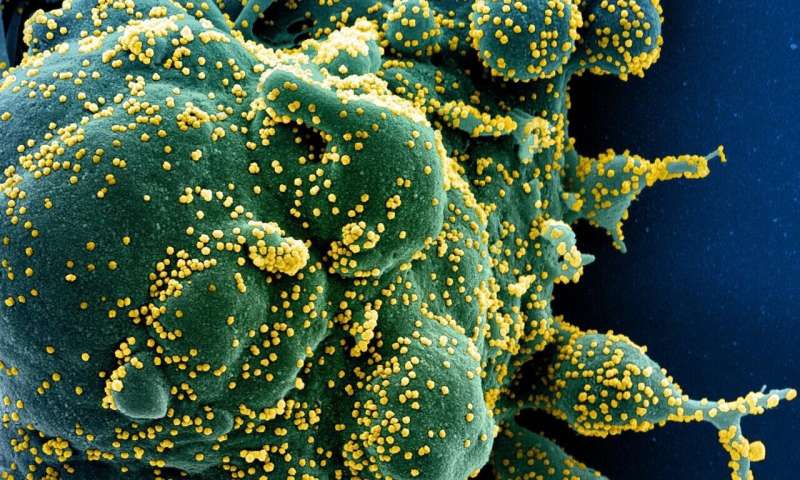
“COVID-19 represents a wide range of systemic problems caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In addition to respiratory failure, many individuals with COVID-19 present with multi-organ clinical complications, including cardiac defects, gastrointestinal symptoms, kidney damage, abnormal liver function, neurological manifestations and a number of metabolic abnormalities,” explains Dr. Chen. “Thus, there is strong need to develop a method to systematically study the impact of SARS-CoV-2 infection on different host tissues.”
This presentation focuses on human pluripotent stem cells (cells that can develop into almost any type of cell) and organoids (clusters of types of cells in lab conditions that mimic the function of a particular organ) to systematically evaluate the processes and cellular response during viral infection and also screen for possible drugs to prevent infection.
“By screening ten different type of cells and organoids, we found that lung, colon, heart, liver, and pancreatic organoids and dopamine neurons can be infected by SARS-CoV-2,” says Dr. Chen. “This work presented the first stem cell model to understand the which organs and cells within those organs can be infected by SARS-CoV-2, which in turn led to a clinical trial to study beta cell function in COVID-19 patients. Work on this study is continuing,” she explains.
Furthermore, Dr. Chen and her colleagues reported the first organoid-based screening study and identified several drug candidates blocking SARS-CoV-2 entry into host cells.
In addition, they performed single-cell RNA-sequencing and confirmed that multiple types of cells in the pancreas (islet cells) were susceptible to SARS-CoV-2. Upon SARS-CoV-2 infection, beta cells showed produced less inulin and more alpha and acinar cell markers. The cells still make insulin, but infection meant the level of insulin they make is much lower. At the same time, the infected beta cells also produce glucose and digestive enzymes, suggesting the virus has the ability to fundamentally change cellular fate (known as cellular transdifferentiation).
“This study demonstrates an example of SARS-CoV-2 infection causing cell fate change, which provides further insight into the pathological mechanisms of COVID-19,” explains Dr. Chen. She discusses that there have been case reports of new onset diabetes several weeks after COVID-19 infection. “It is definitely worth investigating the rate of new onset diabetes patients in this COVID-19 pandemic,” she says.
Dr. Chen’s team has also reported on a mini-heart tissue model to show the damage caused by the body’s own macrophages (cells of the immune system) in attacking heart muscle cells (cardiomyocytes) in patients with COVID-19. This work identified Janus kinase (JAK) inhibitor, which protects cardiomyocytes from macrophage-mediated damage upon SARS-CoV-2 infection. JAK inhibitor has been authorized for emergency use for COVID-19 patients. When exposed to SARS-CoV-2, macrophages secrete IL6 and TNFalpha that damage heart cells through JAK/STAT pathway. JAK inhibitor protects heart cells by blocking these pathways of IL6 and TNFalpha.
Dr. Chen concludes: “Organoids can be used as a powerful model to study the potential of a virus to infect, the host response, immune cell-mediated host damage and, finally, for drug screening.”
Source: Read Full Article
