Sero-epidemiological insights into pathways to COVID-19 immunity
There was a difference in disease burden observed during the initial waves of the COVID-19 pandemic due to different infection rates influenced by factors including the type of occupation, ability to shelter in place, usage of sick leave, access to testing, housing status, and crowded conditions in the neighborhood.
Comorbidities like diabetes and heart disease increase the risk of hospitalization and death due to coronavirus disease (COVID-19). Structural disparities play a role in determining the risk for developing comorbidities like diabetes and heart disease and access to health care for disease management. These may eventually influence COVID-19 outcomes in patients suffering from these conditions.
A number of disparities affect vaccine access and uptake in the United States and globally, including reduced access to technology, low literacy rates, poor access to health care, and insufficient information on the safety and efficacy of vaccines against COVID-19.
Collectively, these disparities may affect the extent of population-level immunity and the burden of COVID-19 in the community. Policymakers should take them into account when determining the impact of new variants, the distribution of booster vaccinations, and the response to diseases such as COVID-19.
Serology which involves the measurement of antibody levels has been a useful tool for determining the levels of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection amongst the population.
A new study posted to the medRxiv* server attempts to utilize serology as a tool to identify disparities in infection rates and vaccination coverage.

Serology as a tool to identify disparities in COVID-19 health care
A serological test allows for the simultaneous measurement of biomarkers representing infection and vaccination in order to correlate them with demographic and geographic factors.
Measurement of long-lived antibody responses to both SARS-CoV-2 spike and non- spike proteins will help understand and segregate immune responses that result from prior infections or vaccinations. It is especially useful in areas where SARS-CoV-2 spike protein-based vaccines are available.
The present study exemplifies the use of serology to understand disparities from a domestic standpoint through a case study in San Francisco.
A serosurveillance platform to quantify disparities in infection rates and vaccination coverage in San Francisco
San Francisco has demonstrated a successful response to COVID-19 and good vaccination coverage in recent months. However, the number of COVID-19 cases and hospitalization rates have been high in areas occupied by socioeconomically low sections of the population, especially among the homeless and the Black and Latinx communities.
Reports show disparities in vaccination coverage in certain vulnerable communities. Despite issues having been addressed vaccinations are still low amongst the homeless and the Black/African Americans.
A SARS-CoV-2 serosurveillance platform was launched in March 2020 with the aim of quantifying the disparities in both infection rates and vaccinations. The platform functions by utilizing the residual blood samples from two hospital networks based in San Francisco. The results from the platform showed that during the first wave of the COVID-19 pandemic seroprevalence in the Latinx individuals was twice as higher than in white individuals. Further, the seroprevalence in homeless individuals was nearly twice as high as the population average.
For the study, samples were collected from subjects during routine blood draws between February 4 and February 2021, which was a period that covered the first 11 months of the pandemic and also the early phase of the vaccine rollout.
These samples were subjected to two serological assays, one specifically detecting SARS-CoV-2 antibodies in response to infections and not due to vaccinations and the other detecting antibodies produced in response to both infection and vaccination.
The study analyzed the test results using Bayesian statistical models and determined the proportion of the population that was seropositive due to natural infection or vaccination and stratified the results based on age, race, and zip codes of residence.
The results from the study revealed that amongst the tested population, 28.2% had any antibodies to SARS-CoV-2, and 8.9% had antibodies due to prior infections.
Disparities exist in infection rates and vaccination coverage in San Francisco
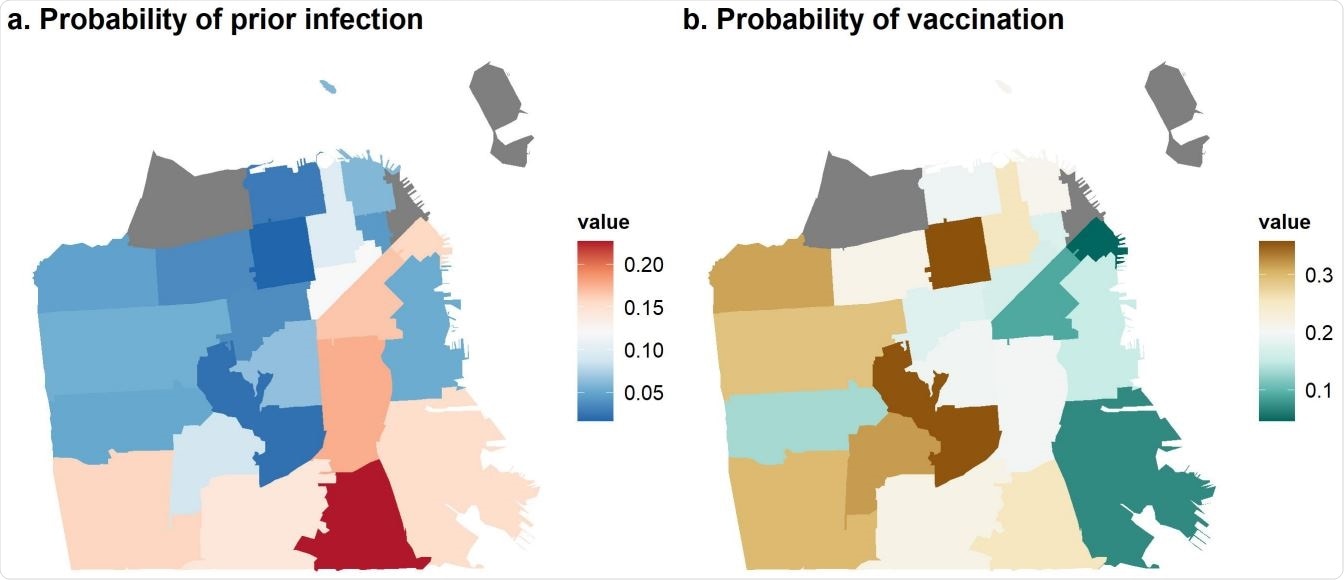
Significant differences were observed in prior infection and vaccination rates in San Francisco. In the Southeastern region of the city, it was found that neighborhoods with no optimum health care access had significantly higher rates of prior infection and lower vaccination rates across all age, demographic groups, and zip codes.
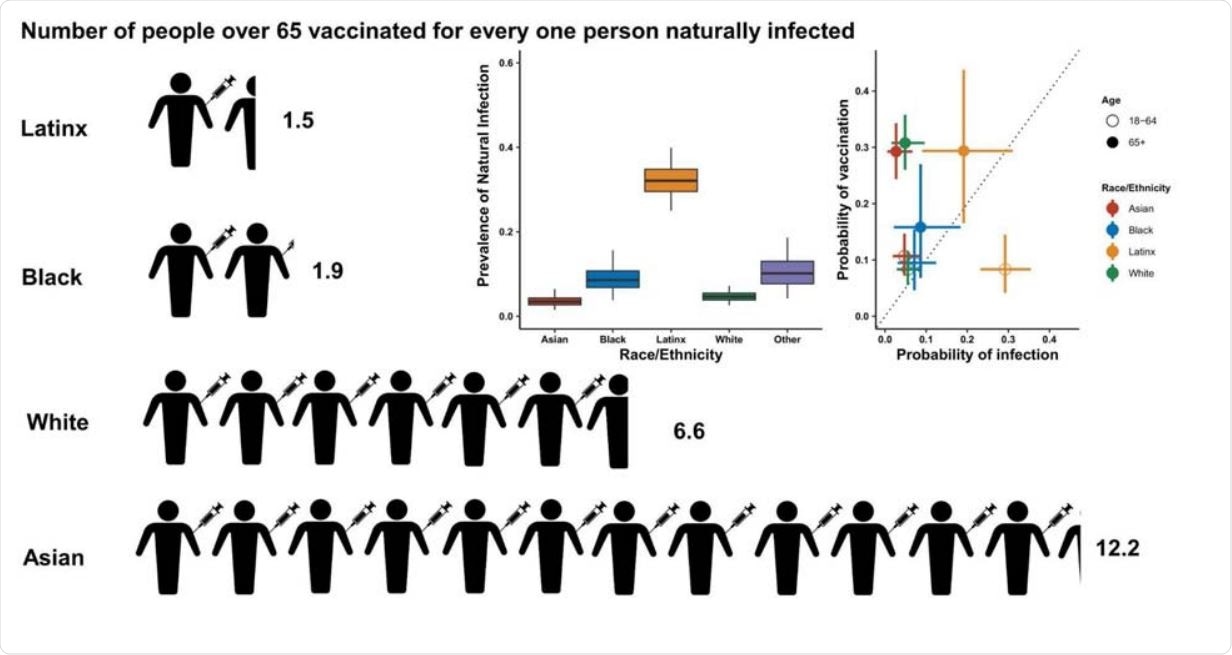
Significant differences in prior infection rates were also detected, which correlated with race/ethnicity. Latinx residents showed 5.4 times more prior infection rates when compared to whites suggesting significant differences in prior infection rates correlated with race/ethnicity.
Disparities were also observed among vaccination rates amongst the population 65 years or older who were eligible for vaccination during the initial vaccine roll-out phase. It was found that white residents who were 65 years and above were twice as likely to be vaccinated as compared to their black counterparts. However, they are half as unlikely to have prior infections, placing them in a position of advantage.
The findings suggest the existence of huge disparities between the risk of infection and vaccination rates amongst specific populations. For example, amongst the population that was 65 years or older, increased ratios of vaccination compared to the risk of infection was found in Asian and white population. In contrast, this ratio was very low in the Black and Latinx population.
Though San Francisco reached 80% vaccine coverage amongst its adult population, recently, high incidence of infections have been reported in neighborhoods that showed the lowest vaccine-related immunity and were also badly hit during the initial infection phase.
A similar finding was also reported in Austin, Texas, where increased COVID-19 cases and decreased vaccination rates correlated with low socio-economic areas and population. Areas populated with Latinx communities which showed higher evidence of deprivation correlated with higher incidences of SARS-CoV-2 infection and low vaccinations. Disparities in SARS-CoV-2 vaccinations in socially vulnerable populations have been documented to be prevalent in the United States and globally.
Addressing upstream and downstream structural drivers of health care disparity to establish health equity
A “double burden” was observed during the early phase of pandemic and vaccine rollout in San Francisco. Structural inequalities exist even in a city like San Francisco that has a good public health care system and social safety nets. Apart from identifying disparities, it is also essential to adopt measures to ensure health equity and vaccine coverage.
In San Francisco, the disparities in vulnerable communities for vaccine coverage was addressed through community-academic partnerships. This partnership helped to effectively respond to the pandemic in communities with a vulnerable population and to narrow the gaps in vaccine coverage by creating low-barrier neighborhood vaccination sites.
As we advance towards the problem of waning immunity against COVID-19 that may require booster doses of vaccines, it becomes essential to establish health equity by addressing the disparities. This will ensure efficient allocation and access to resources and health care amongst populations belonging to different socio-economic strata.
In the United States where vaccinations and COVID-19 infections produce different immune responses, serology will serve as a valuable tool to identify disparities. However, careful consideration should be given to the choice of the assay for the serosurvey as each assay is specific to a pathway, and assays that measure overall antibody prevalence may mask differences in infection rates due to infection and vaccination.
To address the disparities in infection rates and vaccinations amongst the population, policymakers should focus on both the upstream and downstream structural drivers of health care disparity. Some of the upstream structural drivers include providing a living wage to workers, affordable accommodation, access to quality health care.
The downstream drivers of health care disparity include enhanced community engagement, targeted testing and vaccine supply, assistance to overcome barriers to health care like access to technology, access to reliable information in multiple languages, literacy rates, and transportation facilities.
The structural inequalities in health care and other areas affecting a community and a country as a whole should be efficiently addressed in order to effectively combat the COVID-19 pandemic and other similar challenges that may endanger mankind.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Structural inequalities in the pathway to COVID-19 immunity, medRxiv, https://www.medrxiv.org/content/10.1101/2021.10.06.21264573v1
Posted in: Men's Health News | Device / Technology News | Medical Research News | Women's Health News | Disease/Infection News
Tags: Antibodies, Antibody, Assay, Blood, Coronavirus, Coronavirus Disease COVID-19, Diabetes, Efficacy, Health Care, Heart, Heart Disease, Hospital, immunity, Pandemic, Protein, Public Health, Respiratory, SARS, SARS-CoV-2, Serological Test, Serology, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Vaccine

Written by
Dr. Maheswari Rajasekaran
Maheswari started her science career with an undergraduate degree in Pharmacy and later went on to complete a master’s degree in Biotechnology in India. She then pursued a Ph.D. at the University of Arkansas for Medical Sciences in the USA.
Source: Read Full Article



