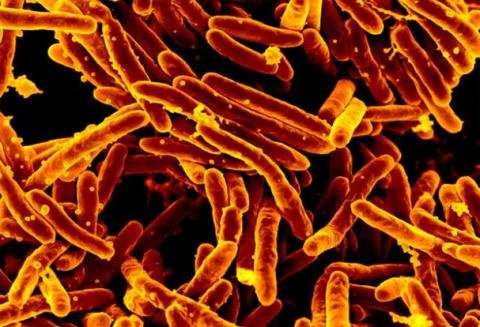
A new all-oral six-month treatment regimen is safer and more effective at treating rifampicin-resistant tuberculosis (RR-TB) than the current accepted standard of care, according to results announced at the 52nd Union World Conference on Lung Health.
These results, which are not yet peer-reviewed, signal the start of a new chapter for people with drug-resistant (DR)-TB who currently face lengthy treatment regimens of up to 20 months that can include painful injections and up to 20 pills a day that can cause severe side-effects. These grueling regimens only cure one in two patients and can have a catastrophic effect on people’s physical and mental health, as well as their financial and social lives.
Carried out by Médecins Sans Frontières/Doctors Without Borders (MSF) with the London School of Hygiene & Tropical Medicine (LSHTM) and other partners, the TB-PRACTECAL trial is the first-ever multi-country, randomized, controlled clinical trial to report on the efficacy and safety of a six-month, all-oral regimen for RR-TB.
It tested a six-month regimen of bedaquiline, pretomanid, linezolid and moxifloxacin (BPaLM), against the locally accepted standard of care. The trial enrolled 552 patients overall, of which 301 were included in the analysis at this stage. The trial took place in seven sites across Belarus, South Africa and Uzbekistan.
The trial researchers are sharing this data with the World Health Organisation (WHO) ahead of the WHO DR-TB treatment guideline review with the hope of influencing national DR-TB guidelines and ultimately clinical practice.
The phase II/III clinical trial found that the new shorter treatment regimen was very effective against RR-TB. 89% of patients in the BPaLM group were cured, compared to 52% in the standard of care group. Tragically four patients died from TB or treatment side effects in the control group, while there were no deaths among patients on the new regimen. Additionally, trial results showed that the new drugs lead to a significantly lower rate of major side effects, with 80% of patients avoiding any major side effects compared to 40% in the control group.
Bern-Thomas Nyang’wa, MSF Medical Director and Chief Investigator of the trial, said: “When we embarked on this journey nine years ago, patients with DR-TB around the world were facing lengthy, ineffective and grueling treatment that disrupted their lives. Patients were telling us how hard it was to adhere to treatment, but little progress was being made to find kinder treatments because diseases most prevalent in low- and middle-income countries don’t attract investment. So we were compelled to pursue new treatment options ourselves. These results will give patients, their families and healthcare workers worldwide, hope for the future of DR-TB treatment.”
Professor David Moore from LSHTM said: “For decades we have treated people with multidrug-resistant TB with long, poorly tolerated drug regimens that have failed to cure half of all patients and have brought dreadful side-effects. This trial shows we can achieve high rates of treatment success, comparable with the outcomes of standard treatment for drug-susceptible TB, without the unbearable toxicity.
“This is the breakthrough that patients and clinicians have hoped for—a drug regimen without months of daily injections that is not only more effective than ‘standard of care’, but is also a much shorter treatment period, fewer drugs and less debilitating side effects.”
Nosipho Ngubane, Principal Investigator at King DinuZulu Hospital, South Africa, one of the seven TB-PRACTECAL trial sites, said: “It has been an honor to serve our communities through this research. For participants, it has been easier to comply with the treatment and complete this shorter regimen which uses fewer tablets.”
The researchers hope these results will serve as a major contribution to the growing body of evidence for global treatment recommendations to be updated to include a short, effective, and safe treatment regimen, as they believe this trial proves that a change in clinical practice is now due.
Awande Ndlovu, who was enrolled in the trial at the THINK Hillcrest Clinical Trial Unit in South Africa, said: “The shorter treatment would mean a lot as I think when you are on treatment, some parts of your life feel like they are put on hold. Before the trial gave me hope, I couldn’t even see the slightest glimpse of recovering from MDR-TB.”
Source: Read Full Article
