Man hospitalized with seizures discovers tapeworm was in brain for decades

Fox News Flash top headlines for November 16
Fox News Flash top headlines are here. Check out what’s clicking on Foxnews.com.
A man hospitalized with mysterious seizures and an “altered mental status” had tapeworms living in his brain for decades, according to researchers.
In a case study published last week in The New England Journal of Medicine, experts from Massachusetts General Hospital and Harvard Medical School said the 38-year-old man was initially evaluated following his first seizure and had been “speaking gibberish.”
The man, who had immigrated from rural Guatemala, was combative and disoriented until he arrived at the hospital, where he had a witnessed generalized tonic-clonic seizure.
Although the patient’s eyes were open – with an involuntary upward gaze – he did not verbally respond to questions or follow commands.
Gag and cough reflexes were normal and the man had no history of illness, medication or drug use and rarely drank alcohol.
The doctors gave him two doses of lorazepam administered intravenously seven minutes apart, and an endotracheal tube was placed for airway protection.
A chest radiograph taken was normal, and the team eventually diagnosed the patient, noting in the study that among patients presenting with an apparent first seizure, obtaining the clinical history is key.
Laboratory testing ruled out hyponatremia, renal dysfunction and liver dysfunction, and the man’s urine and serum toxicology panels were negative. However, further evaluation revealed leukocytosis and lactic acidosis.
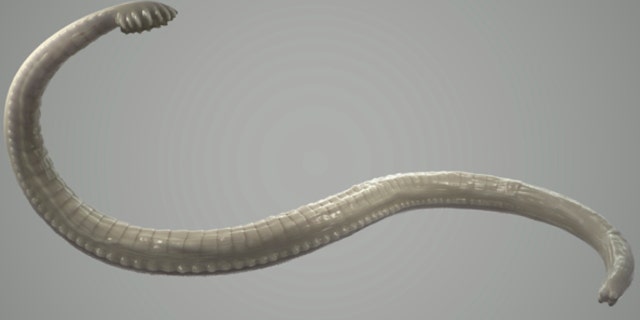
An illustration of a tapeworm
(Credit: iStock)
Although an MRI has higher sensitivity and specificity than a CT scan of the head for the detection of brain parenchymal lesions, a CT is more commonly used in the emergency department
“It is likely that this patient underwent CT after arrival and stabilization in the emergency department, but if the CT study was negative, MRI would ultimately help us to carefully assess for a causative anatomical abnormality,” wrote Dr. Andrew Cole.
Cole also noted that electroencephalography (EEG), which is “extremely useful in classifying the seizure problem,” is also rarely performed rapidly in the emergency department.
Cole wrote that cysticercosis is the most common cause of acquired epilepsy worldwide, resulting from the ingesting of tapeworm eggs.
“On the basis of the features of the patient’s presentation, the fact that he had been healthy the day before the seizure, and his history of living in a rural area of Guatemala, neurocysticercosis is the most likely diagnosis in this case. To establish this diagnosis, CT was most likely performed, followed by MRI and EEG,” Cole said.
During imaging, Dr. George Eng wrote that when findings are suggestive of cysticercosis, the diagnosis can be confirmed with serologic studies.
In testing for anti-cysticercal antibodies with the use of an enzyme-linked immunoelectrotransfer blot (EITB) assay, the presence of those antibodies was negative.
“The patient had evidence of three brain lesions, with one showing ring enhancement on MRI and all three showing partial calcification on CT. The calcifying progression of the lesions may account for the absence of antibody positivity in this patient. In addition, tests for antibodies against toxoplasma, strongyloides, and treponema were negative, as were an interferon-gamma release assay and a purified protein derivative tuberculin skin test for tuberculosis,” Eng said.
The 38-year-old had tested negative for latent tuberculosis – consensus guidelines recommend that patients who will receive prolonged glucocorticoid therapy first be evaluated for latent tuberculosis – and was empirically treated with ivermectin for possible concomitant strongyloidiasis.

The man was admitted to the neurosciences intensive care unit, and his lactic acid level and white-cell count both normalized within hours. Levetiracetam therapy was started to control seizures. An EEG was performed, and the patient was extubated 12 hours after presentation.
He was transferred to the neurology service the following morning and started treatment with two weeks of albendazole and praziquantel, four weeks of high-dose prednisone and a four-week tapering course. He was discharged on hospital day five with no further seizure activity and normal results on a neurologic examination.
The U.S. Centers for Disease Control and Prevention (CDC) notes that humans can become infected with tapeworms by eating raw or undercooked beef.
Living in endemic areas can put people at greater risk, as well as exposure to livestock, poor hygiene and travel, the Mayo Clinic warns.
Source: Read Full Article



