Battle fatigue can drive T cells to exhaustion: Cancer and viruses are tough to fight
Just as it is for marathoners who’ve completed a 26-mile run, or shrubs that have gone without water in a heatwave—exhaustion is an unavoidable fact of life. Dogs get exhausted after herding sheep; birds turn in for the night after an exhausting day of flying and singing. The same is true for T cells, the workhorses of the immune system—they get exhausted, too.
As more investigators turn their attention to this extraordinary phenomenon—T cells too fatigued to function—an international team of investigators foresees the possibility of reversing the exhaustion. The aim is to reinvigorate cellular warriors that have been beaten down by germs or sucker punched by tumor cells and rendered too worn out to fight.
T cell exhaustion refers to their dysfunction, caused by chronic antigen stimulation. Antigens are proteins from infectious agents or tumor cells, recognized by healthy T cells as foreign—and dangerous. Antigens are the reason T cells pull out all the stops as they mount an immune response to eliminate offenders.
Putting up a powerful and sustained response can have disabling, even fatal consequences. T cells react to foreign antigens through their receptors—T cell receptors—or simply, TCRs. The receptors recognize and respond to antigens through potent signaling capabilities. But antigen overstimulation of TCRs—as is common in major persistent infections—can damage T cell signaling and exhaust the TCRs’ ability to respond effectively to threats.
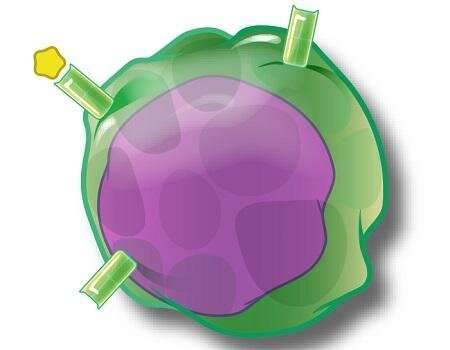
In a joint investigation involving scientists from the United States and Japan, researchers took an in-depth look at T cell exhaustion to find out why and when it occurs. Additionally, they identified a key protein embedded in the T cell surface, a transmembrane protein that serves as a marker of T cell exhaustion. Under conditions of widespread fatigue the transmembrane protein, named Tim-3, singularly signifies T cell exhaustion, the scientists found.
The presence of this transmembrane protein stands as powerful evidence that persistent and overwhelming antigen exposure results in the exhaustion of TCR signaling, even the deletion of vast numbers of T cells. These warriors can become exhausted under the constant pressure of fighting an offender that can’t be easily knocked out.
“Because the transmembrane receptor Tim-3 is increased in abundance on exhausted T cells, it is thought to inhibit T cell activation and is being considered as a therapeutic target to reinvigorate antitumor responses,” wrote Drs. Lawrence P. Kane and Shunsuke Kataoka, authors of a T cell exhaustion study in the journal Science Signaling.
Lane is a researcher at the University of Pittsburgh. Kataoka studied at the university as a graduate student but also is on staff at Asahi Kasei Pharma Corporation in Shizuoka, Japan. They worked with a multi-disciplinary team at the University of Pittsburgh and found that Tim-3 not only serves as a marker for T cell exhaustion, but surprisingly also stimulates some exhausted T cells to resume signaling.
Using various imaging techniques, the international team demonstrated that Tim-3 is recruited to T cell immune synapses, the critical points of contact between T cells and antigen-presenting cells, such as sites of contact with dendritic cells (which literally present T cells with antigens of invaders that have breached the body).
Because of Tim-3’s influence, enhanced signaling can resume downstream for some TCRs. Despite the resumption, it apparently is not enough to reinvigorate armies of exhausted T cells. But now that it’s known how some T cells are revived, it’s theoretically possible to intervene with a pharmaceutical boost.
Investigations into T cell exhaustion are not new research endeavors. Some studies date back nearly 30 years. An animal study from 1993, for example, examined viral persistence in acutely infected, immunocompetent mice. Viral persistence led to exhaustion of antiviral cytotoxic effector T cells, researchers found.
Even though immunologists first described T cell exhaustion occurring in response to chronic viral infection, they found the powerful T cell response to cancers can result in TCR dysregulation, too.
Exhaustion has been well documented in various subpopulations of T cells. A substantial amount of research has been devoted to CD8+ T-cells, particularly the subpopulation known as cytotoxic T cells, which are critical in the destruction of cancerous or virally infected cells. CD4+ T cells also have been shown to develop functional unresponsiveness after chronic infections.
The very act of fighting long-term infiltrators can irrevocably sap the strength of T cells. This is especially true when T cells are caught in a battle royal thwarting infectious diseases of significant public health concern: Hepatitis B and C, or HIV, the human immunodeficiency virus.
Beyond the research by Lane, Kataoka and the team at the University of Pittsburgh, two studies published in the journal Nature Immunology recently drilled down on possible causes of T exhaustion and suggested possible ways to reverse it. And while Lane and Kataoka, suggested that reinvigorating T cells could reboot antitumor responses, a team at Massachusetts General Hospital in Boston, looked into possible rejuvenation of T cells damaged by the persistence of a viral disease.
Dr. Georg M. Lauer of Massachusetts General launched a study that investigated T cell fatigue as a result of hepatitis C infection.
After patients in his study were treated and cured, Lauer and colleagues discovered that exhausted disease-fighting T cells had transformed in ways that made them resemble memory T cells, suggesting antiviral therapy potentially played a role in T cell transformation. Yet, the cells didn’t function as well as genuine memory T cells, the study found.
Lauer said in a statement that “a more superficial study could have been interpreted as real recovery, whereas in reality the key parameters determining the efficacy of a T cell were unchanged.” He added that timing the drug differently may have a stronger impact on sparing T cells.
“We are currently studying whether treating HCV with direct-acting antiviral therapy in the acute phase of infection, instead of many years later, will result in full memory differentiation of T cells. If correct, this could indicate a short window of opportunity early during chronic infections to protect T cell function,” he said.
Source: Read Full Article


